Asthma is a chronic respiratory condition that affects over 300 million people worldwide, and the number is steadily rising. You might know someone who always carries an inhaler, avoids cold weather, or gets breathless during light exercise—it’s often because of Asthma. It doesn’t just affect breathing; it can disrupt daily life, sleep, and even emotional well-being.
At its core, it causes inflammation and narrowing of the airways, making breathing hard. While it isn’t curable, the good news is that it’s highly manageable. With the right treatment plan, medications, and healthy lifestyle adjustments, many people with Asthma lead full, active lives.
In this article, we’ll discuss all about Asthma from symptoms to effective treatment.
What is Asthma?
Asthma is more than occasional shortness of breath—it’s a long-term condition in which the airways become overly sensitive to various triggers. These triggers, such as allergens, cold air, or physical activity, can lead to swelling, tightening of the muscles around the airways, and could also increase mucus production.
The result is a range of symptoms that can flare up suddenly or persist over time. Asthma varies in severity from person to person, but with proper diagnosis and personalized care, symptoms can be kept under control.
Save up to 90% on your medicine bills
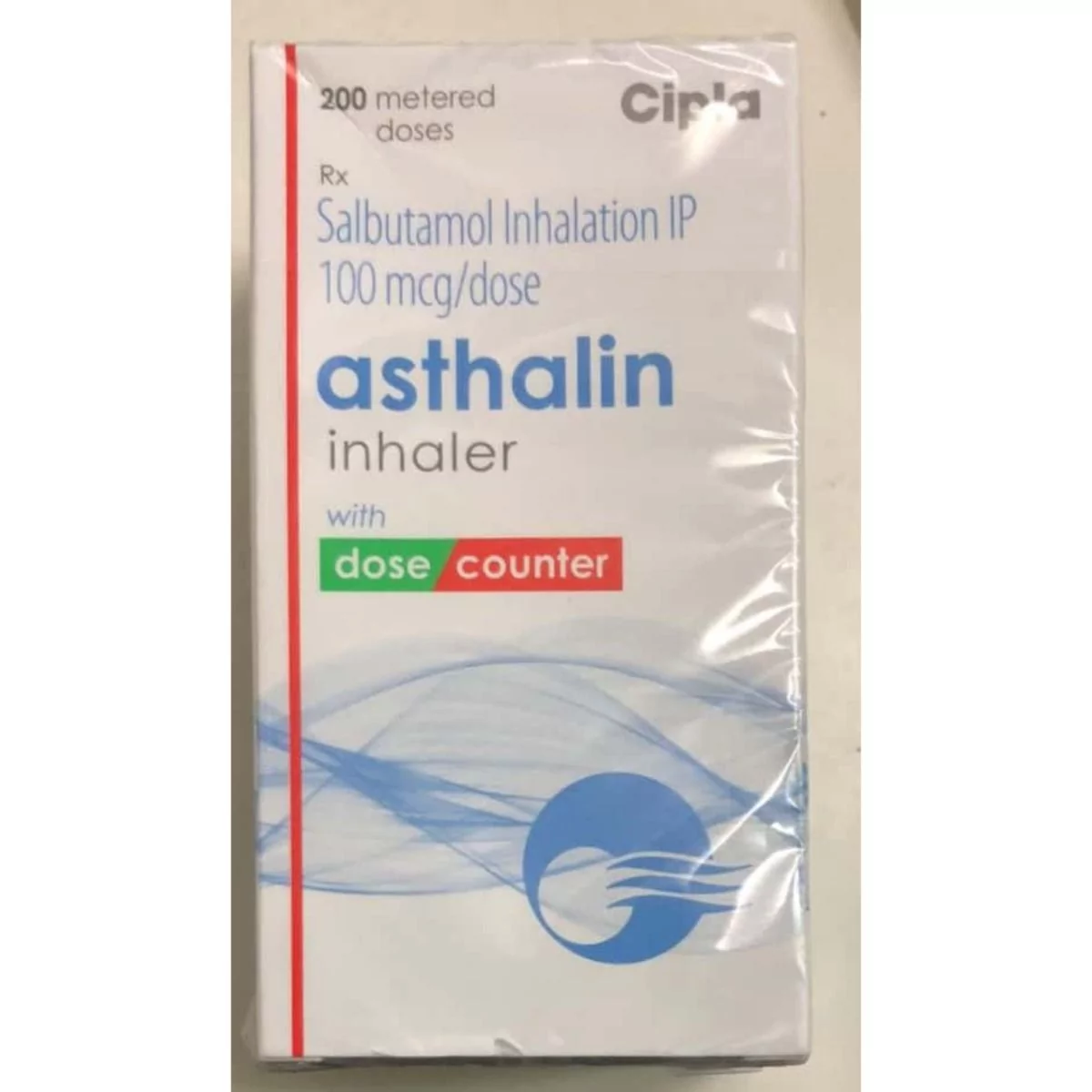
Asthalin 100 mcg Inhaler

Aerocort Inhaler 50 mcg + 50 mcg

Duolin Inhaler 50 mcg + 20 mcg

Asthalin HFA Inhaler 100 mcg (200 mdi)
Asthma symptoms
Asthma symptoms aren’t the same for everyone—they can be mild or more serious. Some people notice them only during exercise or allergies, while others may have them more often. Spotting these signs early helps manage them better and avoid severe flare-ups.
Here are the most common signs and symptoms:
- Shortness of breath
- Wheezing
- Chest tightness or pain
- Persistent coughing
- Difficulty sleeping
- Increased mucus production
Symptoms can worsen with triggers such as cold air, exercise, smoke, allergens, or respiratory infections. If left unmanaged, they can escalate into an Asthma attack—a medical emergency that requires immediate attention.
Types of Asthma
Asthma can show up in different ways depending on what triggers it and how it affects your breathing. Knowing which type you have can help you manage it better. Understanding which kind of Asthma you have helps tailor treatment to address the underlying causes and manage symptoms more effectively. Below are the most common types of Asthma:
Allergic Asthma
This is the most common type, often triggered by pollen, dust mites, pet dander, or mold. It is more common in children and tends to run in families. People with allergic Asthma may also have other allergic conditions like hay fever or Eczema.
Non-allergic Asthma
Unlike allergic Asthma, this type is not triggered by allergens. Instead, it may be provoked by stress, cold air, respiratory infections, or exercise (also known as exercise-induced Asthma). This type is more common in adults and can be harder to diagnose.
Occupational Asthma
This type is triggered by inhaling irritants or allergens at the workplace, such as dust, fumes, chemicals, or mold. It can develop gradually over time and may worsen the longer you’re exposed to the trigger.
Cough-variant Asthma
In this type, the primary symptom is a persistent dry cough, often at night or after exercise, with little or no wheezing or shortness of breath. It can be mistaken for conditions like a common cold or post-nasal drip.
Each type of Asthma can require a slightly different approach to management. Hence, individuals must work closely with their healthcare provider to determine the best course of action based on their type.
What causes Asthma?
Asthma has many possible causes, and experts still don’t fully understand why it develops in some people. However, a mix of genetic and environmental factors plays a significant role. These can trigger symptoms or make them worse. Here are some of the leading causes:
Genetics (Family history)
Asthma tends to run in families. If you have parents or siblings with Asthma or other allergic conditions, you are at a higher risk of developing it yourself. Specific genes related to immune system function and airway inflammation are associated with its development.
Allergens
Exposure to allergens is one of the most common triggers of Asthma, especially in allergic Asthma. Common allergens include:
- Pollen
- Dust mites
- Pet dander
- Mold
- Cockroach droppings
These allergens can irritate the airways and lead to inflammation and constriction, making breathing difficult.
Respiratory infections
Viral infections, particularly in early childhood, may increase the likelihood of developing Asthma later in life. Respiratory infections like the common cold or flu can inflame the airways, making them more sensitive to triggers.

Environmental factors
Being around air pollution, cigarette smoke, or other environmental irritants can raise the risk of getting Asthma or make symptoms worse. People living in cities with much pollution may be more likely to have flare-ups.
Occupational exposures
People who work in environments with dust, chemicals, or fumes—such as construction sites, factories, or farming—may develop occupational Asthma. Exposure to these irritants can inflame the airways and lead to symptoms.
Exercise
Exercise, especially in cold, dry air, can trigger the symptoms in some people. This is known as Exercise-Induced Bronchoconstriction (EIB), where exercise tightens the airways and makes breathing difficult.
Emotional stress and strong emotions
Emotional stress or rapid mood changes can trigger Asthma symptoms. Stress can make you breathe faster, irritating your airways and triggering symptoms.
Hormonal changes
In women, hormonal fluctuations during pregnancy or menstrual cycles can affect Asthma symptoms. Some women may experience worsened symptoms during pregnancy or specific phases of their menstrual cycle.
Knowing these possible causes allows people with Asthma to identify their triggers better and take steps to reduce flare-ups and stay in control of their condition.
Who can get Asthma?
Asthma may affect anyone, regardless of age, gender, or background. While it often begins in childhood, it can also develop in adults and seniors. Understanding certain factors that may increase the risk of developing Asthma can help with early recognition and management.
Here are some common groups at higher risk:
- Children, especially those with a family history of Asthma, allergies, or Eczema.
- People with hay fever or food allergies may be linked to Asthma.
- Individuals are exposed to irritants such as tobacco smoke, air pollution, or workplace chemicals.
- Frequent respiratory infections, especially in early life, may increase the risk of developing Asthma.
- Excess weight can reduce lung function and increase airway inflammation, raising the risk of developing Asthma.
Identifying these risk factors can lead to earlier diagnosis and more effective management.
Asthma treatment
Managing Asthma effectively means controlling symptoms, preventing flare-ups, and improving quality of life. While there’s no cure, it can be managed through medications, lifestyle changes, and regular medical checkups.
The treatment typically includes:
Controller medications: Inhaled corticosteroids are used daily to reduce airway inflammation and prevent symptoms.
Rescue inhalers: Short-acting bronchodilator inhalers like albuterol that offer quick relief during Asthma attacks.
Long-term medications: Options like leukotriene modifiers or biologics for managing moderate to severe Asthma.
Lifestyle management: Avoid triggers (such as allergens, smoke, or pollution), maintain a healthy weight, and exercise carefully.
Asthma action plan: A personalized plan created with your doctor to track symptoms and respond effectively to flare-ups.
Consistent treatment and awareness are key to living well with this condition.
Conclusion
Living with Asthma may seem overwhelming at times, but with the right understanding, support, and treatment, it’s entirely manageable. Recognizing symptoms early, knowing your triggers, and following a personalized action plan can help reduce flare-ups and improve your overall health.
Whether using daily controller medications, having a rescue inhaler handy, or making simple lifestyle adjustments, every step counts toward better breathing. This condition affects people of all ages and backgrounds, but early diagnosis and consistent care make a big difference.
If you or someone you know is experiencing signs of Asthma, don’t wait—talk to a healthcare provider and take control of your respiratory health today.

Frequently Asked Questions
Can Asthma go away?
No, Asthma doesn’t usually go away completely, but symptoms can be controlled with proper treatment and management. Some children may outgrow it, but many people experience symptoms into adulthood. Regular medical follow-up is essential to keep it under control.
How is Asthma diagnosed?
Asthma is diagnosed through a combination of your medical history, a physical exam, and breathing tests like spirometry. These tests measure how well your lungs work and help doctors confirm if your symptoms are due to Asthma or another condition.
How to use an Asthma inhaler?
To use an inhaler, shake it well, place the mouthpiece, and exhale fully. Press the inhaler while breathing in slowly and deeply. Make sure to hold your breath for 10 seconds, then exhale. Repeat if necessary and rinse your mouth afterward.
How to stop Asthma wheezing without an inhaler?
To relieve wheezing without an inhaler, try sitting upright, breathing slowly through your nose, and using pursed-lip breathing. Stay calm, as stress can worsen symptoms. A warm drink, like tea, may also help open airways. If symptoms persist, seek medical attention.
Does Asthma cause chest pain?
Yes, Asthma can cause chest tightness, which may feel like pain. This happens when the airways constrict, making it harder to breathe. However, chest pain unrelated to it may signal other conditions, so it’s essential to consult a doctor for a proper diagnosis.
Cheap Medicine Shop only refers to credible, authoritative sources for our content. If you’re curious about how we ensure the integrity of our content, we encourage you to read our Content Information Policy.














